Note - This is an a online e log book to discuss our patient's de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centred online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment.
DOA - 20/11/23
Case -
A 20 yr old girl came to the GM OPD with complaints of •pain abdomen since 1 day
•vomitings about 8-10 episodes since yesterday night
History of presenting illness -
Patient was apparently alright 4 yrs back then she sustained some injury on her left leg for which she was operated and a rod was inserted. During this time it was discovered that she suffers from high blood sugar levels and was started on insulin since then.
About 1 yr back she visited our hospital with similar complaints of pain abdomen which is increased in intensity on lying down and changing her position. She was then diagnosed to have acute pancreatitis by running some investigations and scanning and was adviced treatment accordingly.
Since 1 yr she is on some anti-diabetic medication as prescribed in Miryalaguda. (Unknown as the patient didn’t bring it along)
Yesterday night she complained of pain in the abdomen in epigastric region which is continuous, more on lying straight and decreased in assuming lateral position. It is non-radiating and dull aching type. The pain is associated with 8-10 episodes of continuous vomitings which is projectile in nature, watery in consistency and non-bilious with no food particles as she did not feel like eating anything that night. She also didn’t take her night dose of medication as she skipped food.She was taken to local RMP and treatment was given after which vomitings subsided.
No h/o loose stools, fever, cough, cold, breathlessness, burning micturition
No h/o chest pain, palpitations, paroxysmal nocturnal dyspnea , pedal edema
No h/o any bleeding manifestations
Past history -
K/c/o DM since 4 yrs took insulin, now on unknown medication since 1 yr
K/c/o pancreatitis since 1 yr
N/k/c/o HTN, TB, asthma, epilepsy, CVA, CAD, thyroid disorders
Personal history -
She is an undergraduate student in some health facility in Miryalaguda.
Wakes up, has breakfast - idly , goes to college.
Has lunch - poori / rice
Comes back at evening and relaxes/ studies.
Has dinner - jonna roti
And goes back to sleep.
Appetite - decreased
Diet - mixed
Bowel - regular
Micturition - normal
Sleep - adequate
No known allergies
No addictions
Family history -
No significant family history
Her grandmother has diabetes
Menstrual history -
Age of menarche - 12 yrs
LMP - 20/11/23
Cycles are regular 28/5 , no pain & no clots
General physical examination -
Pt is conscious, coherent and cooperative and well oriented to time, place and person.
No pallor, icterus, cyanosis, clubbing, lymphadenopathy and edema
Vitals on admission -
Temp - 98F
BP - 100/70 mm hg
PR - 84bpm
RR- 20cpm
Grbs - 377mg/dl
SpO2 - 96% @ RA
Systemic examination -
CVS - S1, S2 heard, no murmurs
RESP SYS - trachea - central , bilateral air entry +, NVBS heard, no added sounds
PER ABDOMEN - soft, tenderness present in the epigastric region, no organomegaly, bowel sounds heard
CNS - NFND
GRBS trends and units of insulin administered-
Pre dinner grbs - 188mg/dl —-> 10 HAI , 8 NPH
2hrs post dinner - 255mg/dl
12am - 175mg/dl
2am - 197mg/dl
4am - 208
6am - 227
Provisional diagnosis-
Diabetic ketosis secondary to non-compliance to medication
K/c/o TYPE 1 DM since 4 yrs
K/c/o pancreatitis since 1.5 yrs secondary to hypertriglyceridemia
Investigations -
ECG

Usg abdomen and pelvis
2d echo
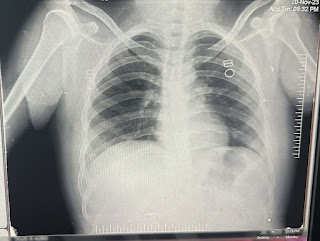
Chest X ray PA view
Final diagnosis -
Diabetic ketosis secondary to non-compliance to medication
K/c/o TYPE 1 DM since 4 yrs
K/c/o pancreatitis since 1.5 yrs secondary to hypertriglyceridemia
Plan of treatment -
Diabetic diet
IV fluids NS and RL @100ml/hr
INJ TRAMADOL 1 amp in 100ml NS IV SOS
INJ PAN 40 mg IV OD
INJ HAI IV INFUSION 40U+39ml NS @ 5 units/hr - increased or decreased according to grbs
Changed to ———->
INJ HAI s/c TID pre-meals (14units-14units-10units)
INJ NPH s/c BD (8units - x - 8 units)
Changed to ————>
INJ HAI s/c BD (15units - x - 10units)
INJ NPH s/c BD (10units - x - 12units)
Tab FENOFIBRATE 160 mg PO OD
Monitor GRBS 7 point profile
Strict I/o charting
OSCE
How is a case of acute pancreatitis diagnosed?
Increased levels of serum amylase and lipase about three times the upper limit of normal value.
Normal S.amylase - 23-85 U/L
S. lipase - 0-160 U/L
Ultrasound or CT evidence of pancreatic swelling
Which is more specific serum amylase or lipase?
Serum lipase has greater diagnostic accuracy as it remains elevated for a longer period of time i.e about 8 to 14 days.
What is the cause of pancreatitis in this case?
The most probable cause of pancreatitis in this case is hypertriglyceridemia.
How does hypertriglyceridemia cause pancreatitis?
The mechanism by which elevated triglyceride levels lead to pancreatitis is not fully understood. A leading hypothesis is that the interaction of high levels of triglyceride rich lipoproteins with pancreatic lipase in the pancreatic capillaries leads to the breakdown of triglycerides to free fatty acids and phospholipids to lysophosphatidylcholine. Both free fatty acids and lysophosphatidylcholine could induce pancreatic damage resulting in pancreatitis. Additionally, the elevated chylomicron levels increase plasma viscosity in the pancreatic capillaries resulting in stasis and hypoxia that can injure the pancreas.
Chylomicronemia may be due to a monogenic disorder (familial chylomicronemia syndrome; FCS) or due to multiple genes (polygenic) in association with other factors (multifactorial chylomicronemia syndrome; MFCS). Greater than 95% of patients with chylomicronemia have MFCS rather than FCS.
What is the cause of diabetic ketosis in this case?
Non-compliance to anti-diabetic medication
Types of diabetes mellitus.
Type 1 DM - juvenile onset - absolute deficiency of insulin due to beta cell destruction
Type 2 DM - adult onset - relative insulin deficiency or insulin resistance - genetic and environmental factors are responsible
Type 3 DM -
A) Genetic defects of beta cell function (MODY)
B) Genetic defects in insulin action
C) Disease of exocrine pancreas
D) Endocrinopathies (acromegaly, Cushing syndrome)
E)Drugs or chemical induced ( eg - nicotinic acid, thiazides)
F) Infections (congenital rubella , cytomegalovirus infection)
G)Uncommon forms of immune mediated diabetes
H) Other genetic syndromes (Down’s syndrome, Klinefelter’s syndrome)
What are the types of insulin?
What diet would you suggest for a diabetes patient?
Diabetic diet -
According to the American Diabetes Association (ADA), a beneficial diet for people with diabetes includes the following:
- fruits and vegetables
- lean protein
- foods with less added sugar
- fewer processed foods
Consumption of whole grains rich in fibres such as brown rice, whole grain bread rather than refined white grains as they have low Glycemic index.
Eat small meals at frequent intervals rather than heavy meals at longer intervals of time.



















Comments
Post a Comment